Some sources, and long lists of references.
How come DEPUTY MINISTER OF HEALTH, MK Litzman, the person highest on the hierarchy of the Ministry of Health of Israel, is NOT taking the H1N1 vaccine?
And how come Bibi, THE MINISTER OF HEALTH, WILL HAVE TO ASK HIS OWN DOCTOR WHETHER TO TAKE IT OR NOT: DOES HE NOT TRUST THE JUDGMENT OF PROFESSOR ENGELHARD?
DOES HE KNOW SOMETHING YOU AND I ARE NOT SUPPOSED TO KNOW, SUCH AS, WHAT AGREEMENT DID THE STATE OF ISRAEL AND THE PHARMACEUTICAL COMPANIES SIGN, WHAT EXACTLY IS IN THAT AGREEMENT; ARE THERE A NUMBER OF SECRET CLAUSES THAT RAISE SOME DOUBT IN HIS MIND?
BIRD'S EYE VIEW ON H1N1; AN ATTEMPT AT COMPREHENSIVE UNDERSTANDING OF THE ENGINEERED PANDEMIC OF 2009
By Daisy J. Stern, MD
10.ADJUVANTS AND TOXIC ADDITIVES:
FIRST OF ALL, MAKE SURE TO WATCH THIS VIDEO, from a former executive at MERCK - CONNECTED TO CSL.
http://www.youtube.com/watch?v=edikv0zbAlU
U.S. to Buy H1N1 Vaccine Components From Four Firms, July 16
The U.S. government signed contracts with four companies worth a total of almost $1 billion to purchase ingredients used to make vaccines against the new H1N1 influenza virus.
Health and Human Services Secretary Kathleen Sebelius said Monday that the department will commit $884 million to buy supplies of two key ingredients for a potential H1N1 vaccine.
The funds will be used to place additional orders for bulk H1N1 antigen and adjuvant on existing contracts with U.S. units of Sanofi-Aventis SA and AstraZeneca PlC, along with GlaxoSmithKline PlC and Novartis AG. In May, the government earmarked $1 billion to spend on vaccine development. The bulk of the additional contracts announced Monday went to Novartis, with a contract worth about $690 million. Sanofi's contract is worth about $61.4 million; Glaxo's totaled $71.4 million, while a contract signed with AstraZeneca's MedImmune unit totals about $61 million.
Antigen is the active ingredient in a vaccine that causes the human body's immune system to develop antibodies that help fight an invading virus. An adjuvant boosts the body's response to a vaccine and could potentially reduce the amount of antigen necessary for the body to recognize and fight a virus.
jennifer.corbett-dooren@dowjones.com
July 29 (Bloomberg) -- Swine flu vaccine makers may rely on a U.S. emergency declaration to use experimental additives made by GlaxoSmithKline Plc and Novartis AG to boost a limited supply of shots that will be available to fight the pandemic.
The ingredients, known as adjuvants, may be added for the first time to flu shots in the U.S. health officials today are meeting to discuss the additives at the U.S. Centers for Disease Control and Prevention in Atlanta, and to recommend who should receive the limited amount of vaccines drugmakers say they will begin delivering in September or October.
The U.S. Health and Human Services Department declared a public health emergency over swine flu in April, and the Food and Drug Administration has the power to allow the use of unapproved medical products during such a crisis. The U.S. has been slow to approve the use of adjuvants because of safety concerns, and for fear of giving Americans an excuse to avoid getting the shots, said John Treanor, a University of Rochester researcher.
"The question is, do you really feel comfortable throwing this new thing into the mix and do you really need to?" said Treanor, a professor of medicine, microbiology and immunology at the school in Rochester, New York. "I myself, if I had to do it, would really wrestle with that decision."
The CDC agreed to pay London-based Glaxo and Novartis, based in Basel, Switzerland, more than $415 million for adjuvants that could be added to the swine flu vaccines, according to a July 13 statement.
Early Production
Adjuvants may not be necessary if enough shots can be produced without them, according to Health and Human Services. That possibility got a boost today from authorities at the CDC, who said 40 million shots of unadjuvanted vaccine may be available in September, earlier than previously reported, with 80 million more doses ready in October.
A safety concern was raised in 2004 when researchers at the University of Florida in Gainesville reported that mice injected with oils used in the adjuvants developed conditions of the type that occur when the body's immune system produces an excessive protective reaction. Similar reactions haven't been seen in humans.
MF59, made by Novartis and sold in Europe, has been given to more than 40 million people, mostly adults, to prevent seasonal flu, according to the company. Glaxo's adjuvant has proven safe and effective in clinical trials with 39,000 people, said Lisa Behrens, a spokeswoman for the company, in an e-mail. Glaxo will conduct more studies and continue to monitor safety after the vaccines are in use, she said.
Emergency Authorization
Under the U.S. health emergency, the FDA may authorize the use of unlicensed vaccines, according to Peper Long, an agency spokeswoman. The FDA convened an advisory committee July 23 to consider what trials are necessary for the vaccines' approval. Advisory committees consist of medical experts who provide guidance to the agency.
Swine flu's full force may reach the U.S. earlier than the typical flu season, according to the CDC. Vaccine makers are racing to make shots by mid-October, when cases are expected to rise in the northern hemisphere, fueled by cooler temperatures and the return of pupils to close quarters of classrooms.
The World Health Organization, based in Geneva, has said the H1N1 influenza, as the pandemic flu is known, is moving with "unprecedented speed." The flu spread farther globally in less than six weeks than previous pandemics have in more than six months, the Geneva-based agency said on its Web site on July 17. Global health authorities have stopped counting the number of cases and the CDC says more than 1 million people Americans have been sickened by the virus.
Egg Yields
The vaccine makers have found it difficult to cultivate the quantities of virus needed for vaccine, as the strain yields 50 percent to 75 percent less antigen, the substance that induces immunity, compared with a typical seasonal flu strain, according to the WHO. The virus didn't initially grow well in eggs, the principal medium used by the industry, vaccine makers said.
In the last week, scientists have been able to improve yields in eggs for the first time, which should ease pressure on manufacturers, Robin Robinson, chief of the Biomedical Advanced Research Development Authority, the U.S. agency in charge of buying the vaccine, said today. A decision on adjuvant use hasn't been made, he said.
Mixing Oil, Water
The adjuvants are mixes of oil and water that -- by stimulating the immune system -- offer a way to boost the body's response to antigen. Adjuvants, whose effectiveness vary by flu strain, may boost the strength of the antigen as much as 10- fold, as was the case with a bird flu vaccine approved in Europe, said Treanor, of the University of Rochester. By adding an adjuvant the same amount of antigen can be used to treat more people, he said.
"Until GlaxoSmithKline and Novartis can show me it won't harm a rat or guinea pig, I think it's a bad idea to give it to humans," Vicky Debold, a registered nurse with a Ph.D. in public health, who is a member of the FDA's advisory committee for reviewing vaccines, said July 27 in an interview.
The U.S. never had to consider the risks of an adjuvant because regular flu vaccines were deemed to have "worked so tremendously well," said Lone Simonsen, research director in the department of global health at George Washington University in Washington.
"We have had a safe experience with the MF59-adjuvanted vaccine in Italy and Spain for many years now," Simonsen said. "That experience we can lean on. That's going to be the best data we have in time for using adjuvanted vaccines."
U.S. Contracts
CSL Ltd., which has a $180 million order to supply bulk H1N1 antigen to the U.S. government, decided against boosting its vaccine with an adjuvant, preferring to use a formulation more closely resembling the seasonal flu shot, said Mary Sontrop general manager of the Melbourne-based company's biotherapies unit.
The U.S. has contracts with five companies to provide flu shots. Novartis, based in Basel, Switzerland, is responsible for 45 percent of the supply, while Sanofi will provide 26 percent and CSL will make 19 percent, said Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases in Bethesda, Maryland, in an interview last week.
The remaining doses will be made by Glaxo and London-based drugmaker AstraZeneca Plc.
To contact the reporters on this story: Tom Randall in New York at trandall6@bloomberg.net; Gary Matsumoto in New York at gmatsumoto@bloomberg.net.
Last Updated: July 29, 2009
LYON, France and SWIFTWATER, Pa., Aug. 7 /PRNewswire/ -- Sanofi Pasteur, the vaccines division of the sanofi-aventis Group (EURONEXT: SAN and NYSE: SNY), announced today the company has submitted to the U.S. Food and Drug Administration (FDA) a supplemental application for licensure of its influenza A(H1N1) 2009 monovalent vaccine. Responding to recent recommendations by the FDA, the company's supplemental application requests the FDA's evaluation of the influenza A(H1N1) 2009 strain change, which is expected to expedite the licensure process for the pandemic vaccine.
"Filing this application is consistent with our commitment to work collaboratively with public health officials in producing a vaccine against the influenza A(H1N1) 2009 virus," said Wayne Pisano, President and Chief Executive Officer of Sanofi Pasteur. "It is essential that we pursue the vaccine licensure pathway made available to us, while at the same time, continue the important clinical studies of our vaccine."
The supplemental application follows recent recommendations by the FDA to evaluate the influenza A(H1N1) 2009 monovalent vaccines using the same regulatory process by which it approves new viral strains contained in the annual seasonal influenza vaccines. Sanofi Pasteur's influenza A(H1N1) 2009 monovalent vaccine supplemental application specifies the evaluation of a non-adjuvanted vaccine.
While these strain change supplements are not required to be supported by new clinical data, immunogenicity and safety data will be made available through clinical studies. Sanofi Pasteur will test the immunogenicity and safety of its influenza A(H1N1) 2009 monovalent vaccine through clinical trials in the U.S., which began August 6. The planned clinical trials will consist of approximately 2,000 subjects and will also evaluate the safety and potential benefits of adding an adjuvant to the pandemic vaccine. More information on the influenza A(H1N1) 2009 vaccine clinical trials is available at www.clinicaltrials.gov.
LYON, France and SWIFTWATER, Pennsylvania, October 31 2005 /PRNewswire/ -- Sanofi pasteur, the vaccines business of the sanofi-aventis Group (NYSE: SNY), has entered into an agreement with Eisai Co., Ltd. to license their novel adjuvant, E6020, for use in the development of new vaccines to treat or prevent human illnesses. E6020 is a chemically synthesized adjuvant that will be tested by sanofi pasteur to determine its ability to enhance the immune response to a broad range of vaccines.
Under the terms of the agreement, Eisai will provide a license to sanofi pasteur to incorporate the E6020 adjuvant for use in vaccines throughout all geographical regions.
To provide a rapid response against the pandemic threat, sanofi pasteur first selected an alum adjuvant for its proven safety characteristics. Other adjuvants are under evaluation with the objective of further increasing immune response generated by the H5N1 vaccine while reducing the amount of antigen needed for vaccination....
Vaccine dose-sparing strategies are discussed among public health experts who benefit from data generated by sanofi pasteur's clinical trial program.
E6020: a synthetic Toll-like receptor 4 agonist as a vaccine adjuvant.
Ishizaka ST, Hawkins LD.
Eisai Research Institute, 4 Corporate Drive, Andover, MA 01742, USA. sally_ishizaka@eri.eisai.com
Safe and cost-effective adjuvants are a critical component to enhance the efficacy of subunit vaccines. Studies have demonstrated that modified natural lipid As derived from enterobacterial lipopolysaccharides, which are agonists of Toll-like receptor 4, are beneficial to vaccine performance. The synthetic phospholipid dimer, E6020, mimics the physicochemical and biological properties of many of the natural lipid As derived from gram-negative bacteria. Similar to its natural counterparts, E6020, which was discovered and developed by Eisai, agonizes Toll-like receptor 4, albeit in an attenuated fashion, eliciting an immunostimulatory response that is conducive to use as a vaccine adjuvant. The derivation of E6020, along with physicochemical properties and in vitro and in vivo studies of immunostimulation and adjuvant activity, are reviewed as a background to its imminent assessment in the clinic.
Basically, what this means is that they have reached the stage of HUMAN GUINEAN PIGS.
And WHICH gram negative bacteria are they talking about?
See below:
AS04:
This molecule is derived from the lipid A portion of Salmonella minnesota Re595 lipopolysaccharide (LPS), considered too toxic itself for use in human vaccines, by removal of a phosphate group and one of its acyl chains.
7/23/09 The NIH's first studies will use flu shots made by France-based Sanofi-Pasteur
and CSL Ltd., which on Wednesday began a much smaller study of its vaccine in its home country of Australia
Complaint filed against the Czech Republic FDA for awarding Baxter a 1.5. billion CZK without open tender.
Also, claims that the adjuvant MF59, AS 03 and AS04, ( used by Novartis and Glaxo) are immunosterilizants.
Baudner BC, Ronconi V, Casini D, Tortoli M, Kazzaz J, Singh M, Hawkins LD, Wack A, O'Hagan DT
Pharm Res. 2009 Jun;26(6):1477-85
"I have focused on the adjuvants made of monophosforyl lipid A (MPL) MF59TM (containing a polysorpate TweenTM 80) or AS03, AS04 also known as squalene in the proposed vaccines, which are immunosterilant or an immunocontraceptive," Daniel Solis writes.
Gajdova M, Jakubovsky J, Valky J.
Institute of Preventive and Clinical Medicine, Limbová, Bratislava.
Delayed effects of neonatal exposure to Tween 80 on female reproductive organs in rats. Food Chem Toxicol. 1993 Mar;31(3):183-90. PMID: 8473002.
"Baby female rats were injected with polysorbate 80 at days 4-7 after birth. It accelerated the maturing of the rats and caused changes to the vagina and womb lining, hormonal changes, ovary deformities and degenerative follicles."
http://www.ncbi.nlm.nih.gov/pubmed/8473002
The Endogenous Adjuvant Squalene Can Induce a Chronic T-Cell-Mediated Arthritis in Rats
Barbro C. Carlson*, Åsa M. Jansson*, Anders Larsson, Anders Bucht and Johnny C. Lorentzen*
http://ajp.amjpathol.org/cgi/content/abstract/156/6/2057
__________________________________________________________
Now, how can WHO claim the adjuvans is harmless:
http://www.who.int/vaccine_safety/topics/adjuvants/squalene/questions_and_answers/en/index.html
when there is clear evidence of its effects provoking AI deseases:
ANTI-SQUALENE ANTIBODIES LINK GULF WAR SYNDROME TO ANTHRAX VACCINE
http://www.autoimmune.com/GWSGen.html
or
"Dr. Jules Freund creator of this oil-based adjuvant warned in 1956 that animals injected with his formulation developed terrible, incurable conditions: allergic aspermatogenesis (stoppage of sperm production), experimental allergic encephalomyelitis (the animal version of MS), allergic neuritis (inflammation of the nerves that can lead to paralysis) and other severe autoimmune disorders.
Source: : Gary Matsumoto, Vaccine A-The Covert Government Experiment That's Killing our Soldiers and Why GI's are Only the First Victims, Kapitola 3. "The Greatest Story Never Told" http://www.vaccine-a.com/excerpt.html"
Daniel Solis, Prague, Czech Republic
Vaccine Adjuvants: Scientific Challenges and Strategic Initiatives
Authors and Disclosures
Ali M. Harandi,1 Gwyn Davies,2 Ole F. Olesen 3
1Department of Microbiology and Immunology, Institute of Biomedicine, The Sahlgrenska Academy, University of Gothenburg, Sweden
2European Adjuvant Advisory Committee, Cardiac and Vascular Sciences, St George's University of London, UK
3Infectious Diseases Unit, DG Research, European Commission, Brussels, Belgium
Disclosure: The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Published: 05/29/2009
1.Abstract and Introduction
2.Recent Advances & Future Scientific Challenges
3.Adjuvant R&D Is Fragmented & Dispersed
4.European & International Initiatives
5.Expert Commentary
6.Five-year View
1.Abstract and Introduction
Abstract
The majority of vaccine antigens currently under investigation represent recombinant molecules or subunits of pathogens with little or no inherent immunostimulatory property. The development of safe and potent immunologic adjuvants that can increase and direct vaccine-specific immunity is, therefore, required urgently. At the same time, the discovery of Toll-like receptors and other innate immune receptors with the ability to bridge innate immune responses and adaptive immunity is offering unprecedented opportunities for the development of novel adjuvants. However, research on vaccine adjuvants has so far received little attention as an independent scientific priority from most of the main research-funding agencies and policy makers. Further, adjuvant research and development is currently spread over a wide number of highly diverse organizations, including large commercial companies, small biotech enterprises as well as publicly funded research organizations and academia. More efforts are, therefore, needed to highlight the importance of vaccine adjuvants on the global research agenda and to encourage collaboration and flow of information between different stakeholders. This article attempts to underline scientific challenges and strategic priorities in the development of vaccine adjuvants for human use.
Introduction
The development and widespread use of vaccines has proven to be one of the most successful public-health interventions, with an unparalleled impact on global health. Starting with the discovery of smallpox vaccine by Edward Jenner in the late 1700s, empirical approaches have been employed to develop vaccines against a variety of diseases caused by infectious agents. Despite significant progress in this enterprise, vaccines to counter several life-threatening diseases, especially those associated with poverty, including HIV/AIDS, malaria and TB, as well as neglected infectious diseases, are not available.
The majority of vaccine antigens presently under investigation represent highly purified recombinant molecules or subunits of pathogens and, hence, they lack many features of the original pathogens, including the inherent immunostimulatory property. Thus, the development of safe and potent immunologic adjuvants and delivery systems that can enhance and direct vaccine-specific immunity is needed. With few exceptions, aluminum salts (alum) are currently the only vaccine adjuvant approved for human use worldwide. Alum is effective at generating a strong antibody response to an antigen with a bias towards a Th2 type of immune response, and, as such, has been widely and effectively used in many vaccines, such as tetanus, diphtheria, pertussis and poliomyelitis vaccines.[1] The mechanism of immunopotentiation by alum involves inflammation and recruitment of antigen-presenting cells, retention of antigen at the injection site, uptake of antigen, dendritic cell maturation, T-cell activation and T-cell differentiation.[2] Although alum adjuvants have proved their efficiency in a large number of applications, some limitations of alum have been reported. Thus, alum failed to confer satisfactory increase of the immune response in certain vaccines, such as typhoid fever and influenza vaccines. Reports have also demonstrated that alum displays limited ability to raise high antibody titers against small-size peptides. Importantly, alum is a poor enhancer of cytotoxic T-cell immunity and Th1 responses, the type of immunity needed to combat several life-threatening infections and cancers.[1,3] This calls for rational design of novel vaccine adjuvants that can establish protective immunity against different diseases, where traditional vaccine technologies have so far failed, through long-lasting antibody- and cell-mediated immune responses. Many products have been proposed as vaccine adjuvants but have been rejected because of safety concerns and research is needed either to understand how to exploit current adjuvants safely or to explore novel products with better safety profiles. However, research and development of vaccine adjuvants has, so far, received little attention as an independent scientific priority from most of the main research-funding agencies and policy makers. We propose that more effort is required to underscore the importance of vaccine adjuvants on the global research agenda and to promote the partnership and flow of information between different stakeholders.
2.Recent Advances & Future Scientific Challenges
Several decades after the introduction of alum, four new adjuvants have now been incorporated into vaccines that are licensed for human use, and this has led to the recognition of adjuvants other than alum. One of these is MF59, an oil-in-water emulsion adjuvant developed by ex-Chiron, now Novartis Vaccines. While MF59 demonstrated satisfactory adjuvant effect with the influenza vaccine Fluad®,[4] it had a limited beneficial effect when used in conjunction with recombinant herpes simplex virus (HSV) type 2 protein for induction of protection against genital herpes in a human vaccine trial.[5] The second new adjuvant is the immunopotentiating reconstituted influenza virosomes, used in the hepatitis A vaccine Epaxal® (Berna Biotech/Crucell).
[6] The other two adjuvants have been developed by GlaxoSmithKline (GSK) Biologicals; AS04 is a component of the hepatitis B virus (HBV) vaccine Fendrix® and of the human papillomavirus (HPV) vaccine Cervarix®, and AS03 is a component of the prepandemic influenza vaccine Prepandrix®.[7,8]
Recent developments in immunology, including the discovery of Toll-like receptors (TLRs) and other innate immune receptors with the capacity to bridge innate and adaptive immunity, have offered new opportunities for the development of immunostimulatory adjuvants.[9,10] Advances in the design of efficient adjuvants based on the use of TLR agonists have been promising (although it should be noted that some of these were in development before the role of TLRs was identified) and some of these have reached advanced human trials and even registration. Monophosphoryl lipid A (MPL), a TLR4 agonist, is included as a component in AS04, the adjuvant system used in Fendrix and Cervarix developed by GSK.[7] This molecule is derived from the lipid A portion of Salmonella minnesota Re595 lipopolysaccharide (LPS), considered too toxic itself for use in human vaccines, by removal of a phosphate group and one of its acyl chains. Mode-of-action studies demonstrated that TLR4 signaling for the closely-related molecule MPLA (removal of the phosphate group but not the acyl chain) is biased towards the adaptor molecule Toll/IL-1 receptor domain containing adaptor protein-inducing IFN-γ (TRIF), compared with its parent LPS that signals through the inflammatory adaptor protein myeloid differentiation factor 88 (MyD88), as well as TRIF.[11] The TRIF pathway generates no overt inflammation/toxicity in the host and this TRIF bias could, at least in part, be responsible for the reduced toxicity. Since the parent S. minnesota LPS itself has been reported to have a TRIF-biased signaling pathway compared with Escherichia coli LPS,[12] it is possible that the MPL adjuvant in Fendrix and Cervarix has similar properties and this could, in part, explain its reduced toxicity. As a word of caution, in spite of the major recent successes with TLR agonists as vaccine adjuvants, it is noteworthy that a recent experimental study demonstrated that, at least under some circumstances, TLR signaling is dispensable for induction of antibody responses by several standard adjuvants.[13]
The use of immunostimulatory molecules as immunopotentiators/vaccine adjuvants raises theoretical safety concerns, owing to the possibility that some might induce overproduction of inflammatory molecules, leading to overt inflammatory reactions or induction of autoimmunity. Recently, human trials with Heplisav™ (developed by Dynavax), which combines hepatitis B antigen with a CpG sequence (ISS 1018), a TLR9 agonist, were halted in response to a serious adverse effect report from a Phase III trial. After receiving two doses of Heplisav, one of the vaccinees was preliminarily diagnosed with Wegener's granulomatosis, an autoimmune disease involving production of antibodies against neutrophils leading to inflammation of the vasculature.[14] By contrast, a recent large integrated analysis of 68,000 participants who received AS04-adjuvanted GSK vaccines, including hepatitis B vaccine as well as HPV-16/18 and HSV vaccines, concluded that participants who received AS04-adjuvanted vaccines or controls demonstrated a low rate of autoimmune disorders, without evidence of an increase in relative risk associated with AS04-adjuvanted vaccines.[15] In conclusion, TLR agonists have a high potential as vaccine adjuvants but the safety of each adjuvant-antigen combination will have to be carefully evaluated. Based on the rapid evolution of this field, it is likely that a new generation of immunomodulatory adjuvants devoid of, or at least with minimal, systemic adverse reactions and local reactogenicity will be forthcoming.
The vast majority of pathogens invade the body through or establish infection in the mucosal tissues, but most vaccines for human use are administered parenterally. Mucosal immunization has recently attracted much interest as a means of generating protective immunity against mucosally transmitted pathogens. Mucosal immunization offers potential advantages over the parenteral vaccination, including reduced risk of transmission of certain types of infectious agents, for example HIV and HBV, and enhanced patient compliance due to ease of administration. However, our understanding of mucosal immunity and the development of mucosal vaccines remains largely incomplete. This is, in part, because it has often proven difficult to induce potent mucosal immunity by mucosal administration of protein antigens and that recovery and functional testing of antibodies present in the mucosal secretions, as well as mucosal T cells, are labor intensive and technically challenging.[16] In fact, only very few mucosal vaccines are presently approved for human use, including oral polio vaccine, oral live-attenuated typhoid vaccine Vivotif® (Berna Biotech/Crucell), oral cholera vaccines Dukoral® (SBL Vaccines/Crucell) and Orochol® (Berna Biotech/Crucell),[17] oral live-attenuated rotavirus vaccines RotaRix® (GSK) and RotaTeq® (Merck),[18] as well as nasal live-attenuated influenza vaccine FluMist® (MedImmune Vaccines, Inc.).[19] It is becoming increasingly clear, however, that the development of a broader range of mucosal vaccines will require the development of safe and effective mucosal adjuvants. Bacterial toxins, such as cholera toxin (CT) and the closely analogous heat-labile enterotoxin (LT) and their derivatives, are commonly used as potent mucosal adjuvants in experimental models. However, their toxicity, associated with an ADP-ribosylating enzymatic activity, has limited their use for human vaccination. In addition, intranasal administration of toxin-based adjuvants is linked to an elevated risk of adverse reactions, such as Bell's palsy, in humans.[20] In spite of this, and underlining the critical effect of the route of administration for safety as well as for efficacy, LT is being developed for transcutaneous immunization against traveller's diarrhea.[21] To circumvent toxicity, new generations of LT and CT mutants have been developed with reduced or no ADP-ribosylating enzymatic activity and, hence, possessing reduced toxicity but significant adjuvanticity,[22] among which LTK63 developed by Novartis Vaccines has reached advanced human trials.[23] Whether this modification will impact on the risk of Bell's palsy remains to be determined. Therefore, the development of safe yet potent mucosal adjuvants for human use remains a priority with high potential impact.
3.Adjuvant R&D Is Fragmented & Dispersed
Vaccines under development increasingly originate from recombinant technologies and, as comprehension of the innate immune system grows, the need for more-effective vaccine adjuvants is expected to rise considerably. The available data on adjuvant safety and efficacy have mostly been generated using a wide variety of protocols, model systems and individual approaches, which makes it difficult or impossible to compare the activity of different adjuvants. At present, no comprehensive overview or comparative studies of adjuvants are available. Each vaccine development project may, therefore, have to perform their own comparison of a large number of adjuvants in order to select the most efficacious ones. Such an exercise is both time-consuming and costly, and may result in the selection of a suboptimal adjuvant, preventing the antigen from exercising its full potential. This could, eventually, result in discontinuation of the vaccine development due to poor performance. The regulatory authorities in both Europe and the USA consider adjuvants as an integral part of the finished vaccine product. Currently, vaccine adjuvants can, therefore, not be licensed in their own right, but only in a specific antigen-adjuvant formulation, which must be proven safe and efficacious. Nevertheless, the EMEA has recently issued a 'Guideline on Adjuvants in Vaccines for Human Use', which includes detailed directions for the testing of safety and efficacy of adjuvants for human use.[24] While it is clear that the properties of individual antigen-adjuvant combinations will always have to be investigated and extrapolation from one combination to another will have to be performed with caution, the establishment of a generally agreed set of standard tests for comparing different vaccine adjuvants would represent a significant step forward.
Despite the fact that novel vaccine adjuvants are drawing new attention from vaccine researchers, it is ironically difficult to access some of the promising new adjuvants for new vaccines. This can be attributed to the fragmented nature of adjuvant research and the fact that many adjuvants are developed within large commercial organizations. Numerous proprietary adjuvants have thus been developed by the private sector but these are not easily accessible for the public sector. For the pharmaceutical groups that have developed new adjuvants, providing them to third parties is often considered a commercial risk that could result in either loss of competitive advantage or the occurrence of adverse events in trials where new adjuvants are not properly used. As a consequence, many adjuvants and scientific data about adjuvants are not available in the public domain.
6.Five-year View
The discovery of TLRs and other innate immune receptors with the ability of connecting innate and adaptive immunity has presented new opportunities for the development of potent vaccine adjuvants. It is, therefore, expected that within the next 5-year period, in addition to the TLR4 agonist MPL, other TLR-based adjuvants will be components of vaccines approved for human use. It is also anticipated that support from the EC and other international research organizations will provide a platform to pool available knowledge regarding adjuvants across sectors and coordinate interaction between the global stakeholders and initiatives for adjuvant research.
From Dr. Mercola
And as if Vaccines Weren't Dangerous Enough on Their Own …
… imagine them turbocharged.
The main ingredient in a vaccine is either killed viruses or live ones that have been attenuated (weakened and made less harmful).
Flu vaccines can also contain a number of chemical toxins, including ethylene glycol (antifreeze), formaldehyde, phenol (carbolic acid) and even antibiotics like Neomycin and streptomycin.
In addition to the viruses and other additives, many vaccines also contain immune adjuvants like aluminum and squalene.
The purpose of an immune adjuvant added to a vaccine is to enhance (turbo charge) your immune response to the vaccination. Adjuvants cause your immune system to overreact to the introduction of the organism you're being vaccinated against.
Adjuvants are supposed to get the job done faster (but certainly not more safely), which reduces the amount of vaccine required per dose, and the number of doses given per individual.
Less vaccine required per person means more individual doses available for mass vaccination campaigns. Coincidentally, this is exactly the goal of government and the pharmaceutical companies who stand to make millions from their vaccines.
Will There Be Immune Adjuvants in Swine Flu Vaccines?
The U.S. government has contracts with several drug companies to develop and produce swine flu vaccines. At least two of those companies, Novartis and GlaxoSmithKline, are using an adjuvant in their H1N1 vaccines.
The adjuvant? Squalene.
According to Meryl Nass, M.D., an authority on the anthrax vaccine,
"A novel feature of the two H1N1 vaccines being developed by companies Novartis and GlaxoSmithKline is the addition of squalene-containing adjuvants to boost immunogenicity and dramatically reduce the amount of viral antigen needed. This translates to much faster production of desired vaccine quantities."[v]
Novartis's proprietary squalene adjuvant for their H1N1 vaccine is MF59. Glaxo's is ASO3. MF59 has yet to be approved by the FDA for use in any U.S. vaccine, despite its history of use in other countries.
Per Dr. Nass, there are only three vaccines in existence using an approved squalene adjuvant. None of the three are approved for use in the U.S.
What Squalene Does to Rats
Oil-based vaccination adjuvants like squalene have been proved to generate concentrated, unremitting immune responses over long periods of time.[vi]
A 2000 study published in the American Journal of Pathology demonstrated a single injection of the adjuvant squalene into rats triggered "chronic, immune-mediated joint-specific inflammation," also known as rheumatoid arthritis.[vii]
The researchers concluded the study raised questions about the role of adjuvants in chronic inflammatory diseases.
What Squalene Does to Humans
Your immune system recognizes squalene as an oil molecule native to your body. It is found throughout your nervous system and brain. In fact, you can consume squalene in olive oil and not only will your immune system recognize it, you will also reap the benefits of its antioxidant properties.
The difference between "good" and "bad" squalene is the route by which it enters your body. Injection is an abnormal route of entry which incites your immune system to attack all the squalene in your body, not just the vaccine adjuvant.
Your immune system will attempt to destroy the molecule wherever it finds it, including in places where it occurs naturally, and where it is vital to the health of your nervous system.[viii]
Gulf War veterans with Gulf War Syndrome (GWS) received anthrax vaccines which contained squalene.[ix] MF59 (the Novartis squalene adjuvant) was an unapproved ingredient in experimental anthrax vaccines and has since been linked to the devastating autoimmune diseases suffered by countless Gulf War vets.[x]
The Department of Defense made every attempt to deny that squalene was indeed an added contaminant in the anthrax vaccine administered to Persian Gulf war military personnel – deployed and non-deployed – as well as participants in the more recent Anthrax Vaccine Immunization Program (AVIP).
However, the FDA discovered the presence of squalene in certain lots of AVIP product. A test was developed to detect anti-squalene antibodies in GWS patients, and a clear link was established between the contaminated product and all the GWS sufferers who had been injected with the vaccine containing squalene.
A study conducted at Tulane Medical School and published in the February 2000 issue of Experimental Molecular Pathology included these stunning statistics:
" … the substantial majority (95%) of overtly ill deployed GWS patients had antibodies to squalene. All (100%) GWS patients immunized for service in Desert Shield/Desert Storm who did not deploy, but had the same signs and symptoms as those who did deploy, had antibodies to squalene.
In contrast, none (0%) of the deployed Persian Gulf veterans not showing signs and symptoms of GWS have antibodies to squalene. Neither patients with idiopathic autoimmune disease nor healthy controls had detectable serum antibodies to squalene. The majority of symptomatic GWS patients had serum antibodies to squalene."[xi]
ADDENDUM
According to Dr. Viera Scheibner, Ph.D., a former principle research scientist for the government of Australia:
"… this adjuvant [squalene] contributed to the cascade of reactions called "Gulf War Syndrome," documented in the soldiers involved in the Gulf War.
The symptoms they developed included arthritis, fibromyalgia, lymphadenopathy, rashes, photosensitive rashes, malar rashes, chronic fatigue, chronic headaches, abnormal body hair loss, non-healing skin lesions, aphthous ulcers, dizziness, weakness, memory loss, seizures, mood changes, neuropsychiatric problems, anti-thyroid effects, anaemia, elevated ESR (erythrocyte sedimentation rate), systemic lupus erythematosus, multiple sclerosis, ALS (amyotrophic lateral sclerosis), Raynaud's phenomenon, Sjorgren's syndrome, chronic diarrhoea, night sweats and low-grade fevers."[xii]
Post Vaccination Follow-Up Might as Well Be Non-Existent
There is virtually no science to support the safety of vaccine injections on your long-term health or the health of your children. Follow-up studies last on average about two weeks, and look only for glaring injuries and illnesses.
Autoimmune disorders like those seen in Gulf War Syndrome frequently take years to diagnose due to the vagueness of early symptoms. Complaints like headaches, fatigue and chronic aches and pains are symptoms of many different illnesses and diseases.
Don't hold your breath waiting for vaccine purveyors and proponents to look seriously at the long-term health consequences of their vaccination campaigns.
ADVERSE EFFECTS OF ADJUVANTS IN VACCINES
by Viera Scheibner, Ph.D. Ó 2000
Nexus Dec 2000 (Vol 8, No1) & Feb 2001 (Vol 8, Number 2)
ADJUVANTS, PRESERVATIVES AND TISSUE FIXATIVES IN VACCINES
ADJUVANTS
Oil emulsions
Freund's emulsified oil adjuvants (complete and incomplete)
Arlacel A
Mineral oil
Emulsified peanut oil adjuvant (adjuvant 65)
Mineral compounds
Bacterial products
Bordetella pertussis
Corynebacterium granulosumderived P40 component
Lipopolysaccharide
Mycobacteriwn and its components
Cholera toxin
Liposomes
Immunostimulating complexes (ISCOMs)
Other adjuvants: Squalene
IMMUNOLOGY PRINCIPLES: ANTIBODY RESPONSE
IMMUNOPATHOLOGY OF HYPERSENSITIVITY REACTIONS:
Immediate Hypersensitivity
Arthus-type Reaction
Anaphylaxis
Atopy
Delayed Hypersensitivity
Isoimmunological Disease
Immunological Disease Resulting from Adsorption of Foreign Substances
Autoimmune Disease
VACCINATION: A SAFETY WARNING
ADJUVANTS, PRESERVATIVES AND TISSUE FIXATIVES IN VACCINES
Vaccines contain a number of substances which can be divided into the following groups:
1. Micro-organisms, either bacteria or viruses, thought to be causing certain infectious diseases and which the vaccine is supposed to prevent. These are whole-cell proteins or just the broken-cell protein envelopes, and are called antigens.
2. Chemical substances which are supposed to enhance the immune response to the vaccine, called adjuvants.
3. Chemical substances which act as preservatives and tissue fixatives, which are supposed to halt any further chemical reactions and putrefaction (decomposition or multiplication) of the live or attenuated (or killed) biological constituents of the vaccine.
All these constituents of vaccines are toxic, and their toxicity may vary, as a rule, from one batch of vaccine to another.
In this article, the first of a two-part series, we shall deal with adjuvants, their expects role and the reactions (side effects).
ADJUVANTS
The desired immune response to vaccines is the production of antibodies, and this is enhanced by adding certain substances to the vaccines. These are called adjuvants (from the Latin adjuvare, meaning "to help").
The chemical nature of adjuvants, their mode of action and their reactions (side effect) are highly variable. According to Gupta et al. (1993), some of the side effects can be ascribed to an unintentional stimulation of different mechanisms of the immune system whereas others may reflect general adverse pharmacological reactions which are more less expected.
There are several types of adjuvants. Today the most common adjuvants for human use are aluminium hydroxide, aluminium phosphate and calcium phosphate. However, there are a number of other adjuvants based on oil emulsions, products from bacteria (their synthetic derivatives as well as liposomes) or gram-negative bacteria, endotoxins, cholesterol, fatty acids, aliphatic amines, paraffinic and vegetable oils. Recently, monophosphoryl lipid A, ISCOMs with Quil-A, and Syntex adjuvant formulations (SAFs) containing the threonyl derivative or muramyl dipeptide have been under consideration for use in human vaccines.
Chemically, the adjuvants are a highly heterogenous group of compounds with only one thing in common: their ability to enhance the immune response—their adjuvanticity. They are highly variable in terms of how they affect the immune system and how serious their adverse effects are due to the resultant hyperactivation of the immune system.
The mode of action of adjuvants was described by Chedid (1985) as: the formation of a depot of antigen at the site of inoculation, with slow release; the presentation of antigen immunocompetent cells; and the production of various and different lymphokines (interleukins and tumour necrosis factor).
The choice of any of these adjuvants reflects a compromise between a requirement for adjuvanticity and an acceptable low level of adverse reactions.
The discovery of adjuvants dates back to 1925 and 1926, when Ramon (quoted by Gupta et al., 1993) showed that the antitoxin response to tetanus and diphtheria was increased by injection of these vaccines, together with other compounds such as agar, tapioca, lecithin, starch oil, saponin or even breadcrumbs.
The term adjuvant has been used for any material that can increase the humoral or cellular immune response. to an antigen. In the conventional vaccines, adjuvants are used to elicit an early, high and long-lasting immune response. The newly developed purified subunit or synthetic vaccines using biosynthetic, recombinant and other modern technology are poor immunogens and require adjuvants to evoke the immune response.
The use of adjuvants enables the use of less antigen to achieve the desired immune response, and this reduces vaccine production costs. With a few exceptions, adjuvants are foreign to the body and cause adverse reactions.
Part 1 deals with the following types of adjuvants (after Gupta et al, 1993):
Oil emulsions
Freund's emulsified oil adjuvants (complete and incomplete)
Arlacel A
Mineral oil
Emulsified peanut oil adjuvant (adjuvant 65)
Mineral compounds
Bacterial products
Bordetella pertussis
Corynebacterium granulosumderived P40 component
Lipopolysaccharide
Mycobacteriwn and its components
Cholera toxin
Liposomes
Immunostimulating complexes (ISCOMs)
Other adjuvants
Squalene
Oil Emulsions
In the 1960s, emulsified water-in-oil and water-in-vegetable-oil adjuvant preparations used experimentally showed special promise in providing exalted "immunity" of long duration (Hilleman, 1966). The development of Freund's adjuvants emerged from studies of tuberculosis. Several researchers noticed that immunological responses in animals to various antigens were enhanced by introduction into the animal of living Mycobacterium tuberculosis. In the presence of Mycobacterium, the reaction obtained was of the delayed type, transferrable with leukocytes. Freund measured the effect of mineral oil in causing delayed-type hypersensitivity to killed mycobacteria. There was a remarkable increase in complement-fixing antibody response as well as in delayed hypersensitivity reaction.
Freund's adjuvant consists of a water-in-oil emulsion of aqueous antigen in paraffin (mineral) oil of low specific gravity and low viscosity. Drakeol 6VR and Arlacel A (mannide monooleate) are commonly used as emulsifiers.
There are two Freund's adjuvants: incomplete and complete. The incomplete Freund's adjuvant consists of water-in-oil emulsion without added mycobacteria; the complete Freund's adjuvant consists of the same components but with 5 mg of dried, heat-killed Mycobacterium tuberculosis or butyricum added.
The mechanism of action of Freund's adjuvants is associated with the following three phenomena:
1. The establishment of a portion of the antigen in a persistent form at the injection site, enabling a gradual and continuous release of antigen for stimulating the antibody;
2. The provision of a vehicle for transport of emulsified antigen throughout the lymphatic system to distant places, such as lymph nodes and spleen, where new foci of antibody formation can be established; and,
3. Formation and accumulation of cells of the mononuclear series which are appropriate to the production of antibody at the local and distal sites.
The pathologic reaction to the Freund's adjuvants starts at the injection site with mild erythema and swelling followed by tissue necrosis, intense inflammation and the usual progression to the formation of a granulomatous lesion. Scar and abscess formation may occur. The reactions observed following the administration of the complete adjuvant are generally far more extensive than with the incomplete adjuvant. The earliest cellular response is polymorphonuclear, then it changes into mononuclear and later includes plasmocytes. The adjuvant emulsion may be widely disseminated in varrious organs, depending on the route of inoculation, with the development of focal granulomatous lesions at distal places. Various gram-negative organisms may show a potentiating effect of the adjuvant, similar to that displayed by mycobacteria.
The earliest use of oil emulsion adjuvants was made with the influenza, vaccine by Friedwald (1944) and by Henle and Henle (1945). Following their promising results on animals, Salk (1951) experimented with such adjuvants on soldiers under the auspices of the US Armed Forces Epidemiological Board. He used a highly refined mineral oil, and developed a purified Arlacel A emulsifier which was free of toxic substances, such as oleic acid which had caused sterile abscesses at the injection site, and he administered the vaccine by intramuscular route.
Subsequently, Miller et al. (1965) reported their, failure to enhance the antibody and protective response to types 3, 4 and 7 adenovirus vaccines in mineral oil adjuvant compared with aqueous vaccine. Unpublished studies have revealed the need for an adequate minimal amount of antigen to trigger an antibody response to the emulsified preparations.
Salk et al. (1953) applied Freund's adjuvant to poliomyelitis vaccine, and later followed with extensive testing of killed crude as well as purified polio virus vaccine in animals and humans, where the reactions in humans were considered inconsequential.
Grayston et al. (1964) reported highly promising results with the trachoma vaccine using an oil adjuvant. However, the trachoma vaccine lost its relevance because, as demonstrated by Dolin et al. (1997) in their 37 years of research in a sub-Saharan village, the dramatic fall in the disease occurrence was closely connected with improvements in sanitation, water supply, education and access to health care. According to Dolin et al. (1997), the decline in trachoma occurred without any trachoma-specific intervention.
Allergens in Freund's adjuvant deserve special attention because they can be dangerous. These dangers include an overdose, i.e., the immediate release of more than the tolerated amount of properly emulsified vaccine in sensitive persons, or the breaking of the emulsion with the release of all or part of the full content of the allergen within a brief period of time. Long-term delayed reactions include the development of nodules, cysts or sterile abscesses requiring surgical incision. It is also likely that some allergens used, such as house dust or mould, might have acted like mycobacteria to potentiate the inflammatory response. Such reactions have been reduced with the use of properly tested and standardised reagins.
One must also consider that the first application of Freund's adjuvants was made at a time when modern concepts of safety were non-existent Indeed, mineral oil adjuvants have not been approved for human use in some countries, including the USA.
Mineral Compounds
Aluminium phosphate or aluminium hydroxide (alum) are the mineral compounds most commonly used as adjuvants in human vaccines. Calcium phosphate is another adjuvant that is used in many vaccines. Mineral salts of metals such as cerium nitrate, zinc sulphate, colloidal iron hydroxide and calcium chloride were observed to increase the antigenicity of' the toxoids, but alum gave the best results.
The use of alum was applied more than 70 years ago by Glenny et al. (1926), who discovered that a suspension of alum-precipitated diphtheria toxoid had a much higher immunogenicity than the fluid toxoid. Even though a number of reports stated that alum-adjuvanted vaccines were no better than plain vaccines (Aprile and Wardlaw, 1966), the use of alum as an adjuvant is now well established. The most widely used is the antigen solution mixed with pre-formed aluminium hydroxide or aluminium phosohate under controlled conditions. Such vaccines are now called aluminium-adsorbed or aluminium-adjuvanted. However, they are difficult to manufacture in a physico-chemically reproducible way, which results in a batch-to-batch variation of the same vaccine. Also, the degree of antigen absorption to the gels of aluminium phosphate and aluminium hydroxide varies. To minimise the variation and avoid the non-reproducibility, a specific preparation of aluminium hydroxide (Alhydrogel) was chosen as the standard in 1988 (Gupta et al., 1993).
The aluminium adjuvants allow the slow release of antigen, prolonging the time for interaction between antigen and antigen-presenting cells and lymphocytes. However, in some studies, the potency of adjuvanted pertussis vaccines was more than that of the plain pertussis vaccines, while in others no effect was noted. The serum agglutinin titres, after vaccination with adjuvanted pertussis vaccines, were higher than those of the plain vaccines, with no difference in regard to protection against the disease (Butler et al., 1962). Despite these conflicting results, aluminium compounds are universally used as adjuvants for the DPT (diphtheriapertussis-tetanus) vaccine. Hypersensitivity reactions following their administration have been reported which could be attributed to a number of factors, one of which is the production of IgE along with IgG antibodies.
It was suggested that polymerased toxoids, such as the so-called glutaraldehyde-detoxifled purified tetanus and diphtheria toxins, should be used instead of aluminium compounds. They are used combined with glutaraldehyde-inactivated pertussis vaccine.
Calcium phosphate adjuvant has been used for simultaneous vaccination with diphtheria, pertussis, tetanus, polio, BCG, yellow fever, measles and hepatitis B vaccines and with allergen (Coursaget et al., 1986). The advantage of this adjuvant has been seen to be that it is a normal constituent of the body and is better tolerated and absorbed than other adjuvants. It entraps antigens very efficiently and allows slow release of the antigen. Additionally, it elicits high amounts of IgG-type antibodies an much less of IgE-type (reaginic) antibodies.
Bacterial Products
Micro-organisms in bacterial infections and the administration of vaccines containing whole killed bacteria and some metabolic products and components of various micro-organisms have been known to elicit antibody response and act as immunostimulants. The addition of such micro-organisms and substances into vaccines augments the immune response to other antigens in such vaccines.
The most commonly used micro-organisms, whole or their parts, are Bordetella pertussis components, Corenybacterium derived P40 component, cholera toxin and mycobacteria.
•B. pertussis components
The killed Bordetella pertussis has a strong adjuvant effect on the diptheria and tetanus toxoids in the DPT vaccines. However, there are a number of admitted and well-describe reactions to it, such as convulsion, infantile spasms, epilepsy, sudden infant death syndrome (SIDS), Reye syndrome, Guilain-Barre syndrome, transverse myelitis and cerebral ataxia. Needless to say, the causal link to it is often (even though not always) vehemently disputed and generally considered "coincidental".
Paradoxically, in one case of shaken baby syndrome in which the baby developed subdural and retinal haemorrhages from the disease whooping cough, doctors accused the father of causing these injuries and strenuously denied that the disease pertussis can and does cause such haemorrhages—forgetting that this is the very reason why pertussis vaccine was developed against such potentially devastating disease in the first place. Such devastating effects are caused by the pertussis toxin, the causative agent of the disease (pertussis is a toxin-mediated disease), employed as the active ingredient in all pertussis vaccines whether whole-cell or acellular (Pittman, 1984).
Gupta et al. (1993) concluded that PT is too toxic to be administered to humans, but chemically detoxified or genetically inactivated PT may not exhibit the adjuvant effects comparable to the native PT.
•Corynebacterium-derived P40
P40 is a particulate fraction isolated from Corynebacterium granulosum, composed of the cell wall peptidoglycan associate with a glycoprotein. In animals, it displays a number of activities such as stimulation of the reticulo-endothelial system, enhancement of phagocytosis and activation of macrophages.
P40 abolishes drug-induced immunosuppression and increase non-specific resistance to bacterial, viral, fungal and parasitic infections. It induces the formation of IL-2, tumour necrosis factor, and interferon alpha and gamma (Bizzini et al., 1992). In clinical trials, P40 was claimed to be efficacious in the treatment of recurrent infections of the respiratory and genito-urinary tracts. Allergens coupled to P40 have been said to be instrumental in desensitising allergic patients without any side effects.
•Lipopolysaccharide (LPS)
LPS is an adjuvant for both humoral and cell-mediated immunity. It augments the immune response to both protein and polysaccharide antigens. It is too toxic and pyrogenic, even in minute doses, to be used as an adjuvant in humans.
•Mycobacterium and its components
Interestingly, Mycobacterium and its components, as originally formulated, were too toxic to be used as adjuvants in humans. However, the efforts to detoxify them resulted in the development of N-acetyl muramyl-L-alanyl-D-isoglutamine, or muramyl dipeptide (MDP). When given without antigen, it increased nonspecific resistance against infections with bacteria, fungi, parasites, viruses, and even against certain tumours (McLaughlin et al., 1980). However, MDPs are potent pyrogens (maybe that's why they may be effective against certain tumours—my comment) and their action is not completely understood; hence they are not acceptable for use in humans.
•Cholera Toxin
A major drawback with cholera toxin as a mucosal adjuvant is its intrinsic toxicity.
Liposomes
Liposomes are particles made up of concentric lipid membranes containing phospholipids and other lipids in a bilayer configuration separated by aqueous compartments. They have been used parenterally in people as carriers of biologically active substances (Gregoriadis, 1976) and considered safe.
Immunostimulating complexes (ISCOMs)
ISCOMs (DeVries et al., 1988; Morein et al., 199&, Lovgren : al., 1991) represent an interesting approach to stimulation of the humoral and cell-mediated immune response towards amphipathic antigens. It is a relatively stable but non-covalently-bound complex of saponin adjuvant Quil-A, cholesterol and amphipathic antigen in a molar ratio of approximately 1:1:1. The spectrum of viral capsid antigens and non-viral amphipathic antigens of relevance for human vaccination, incorporated into ISCOMs, comprises influenza, measles, rabies, gp340 from EB-virus, gp120 from HIV, Plasmodium falciparum and Trypanosoma cruzi.
ISCOMs have been shown to induce cytotoxic T-lymphocyte (CTL). Following oral administration, some types of CTLs were found in mesenteric lymph nodes and in the spleen, and specific IgA response could be induced.
ISCOMs have only been used in veterinary vaccines, partly due to their haemolytic activity and some local reactions all reflecting the detergent activity of the Quil-A molecule.
Other Adjuvants: Squalene
Squalene is an organic polymer with some antigenic epitopes which might be shared with other organic polymers acting as immunostimulators. It has been used in experimental vaccines since 1987 (Asa et aL, 2000) and it was used in the experiments vaccines given to a great number of the participants in the Gulf War. These included those who were not deployed but received the same vaccines as those who were deployed.
The adjuvant activity of non-ionic block copolymer surfactants was demonstrated when given with 2% squalene-in-water emulsion. However, this adjuvant contributed to the cascade of reactions called "Gulf War syndrome", documented in the soldiers involved in the Gulf War. The symptoms they developed included arthritis, fibromyalgia, lymphadenopathy, rashes, photosensitive rashes, malar rashes, chronic fatigue, chronic headaches, abnormal body hair loss, non-healing skin lesions, aphthous ulcers, dizziness, weakness, memory loss, seizures, mood changes, neuropsychiatric problems, anti-thyroid effects, anaemia, elevated ESR (erythrocyte sedimentation rate), systemic lupus erythematosus, multiple sclerosis, ALS (amyotrophic lateral sclerosis), Raynaud's phenomenon, Sjorgren's syndrome, chronic diarrhoea, night sweats and low-grade fevers.
This long list of reactions shows just how much damage is done by vaccines, particularly when potentiated by powerful "immunoenhancers" such as squalene and other adjuvants. Interestingly, vaccinators as a rule consider such problems as mysterious and/or coincidental with vaccines. Since the administration of a multitude of vaccines to the participants (and prospective participants) in the Gulf War is well-documented (in fact, veterans claim they were given many more than were even recorded), this list of observed reactions further incriminates the vaccines as causing such problems.
IMMUNOLOGY PRINCIPLES: ANTIBODY RESPONSE
To explain the action of adjuvants, we should look into immunology. The theory of vaccine efficacy is based on the ability of vaccines to evoke the formation of antibodies. This is of varying efficacy, depending on the nature of the antigen(s) and the amount of antigenic substance administered.
However, the mechanisms for the diversity of immune reactions are complex, and to this day are not quite known and understood. There are numerous theories, the favoured one being antibody response as the sign of immunisation (acquiring immunity).
Specific immunity to a particular disease is generally considered to be the result of two kinds of activity: the humoral antibody and the cellular sensitivity.
The ability to form antibodies develops partly in utero and partly after birth in the neonatal period. In either case, immunological competence—the ability to respond immunologically to an antigenic stimulus—appears to originate with the thymic activity.
The thymus initially consists largely of primitive cellular elements which become peripheralised to the lymph nodes and spleen. These cells give rise to lymphoid cells, resulting in the development of immunological competence. The thymus may also exert a second activity in producing a hormqne-lilce substance which is essential for the maturation of immunological competence in lymphoid cells. Such maturation also takes place by contact with thymus cells in the thymus.
Stimulation of the organism by antigen results in proliferation of cells of the lymphoid series accompanied by the formation of immunocytes, and this leads to the antibody production. Certain lymphocytes and possibly reticulum cells may be transformed into immunoblasts, which develop into immunologically active ("sensitised") lymphocytes and plasmocytes (plasma cells). Antibody formation is connected with plasma cells, while cellular immunity reactions are mainly lymphocytic.
None of the theories for antibody formation comprehends all the biological and chemical data now available. However, several principal theories have been considered at length.
The so-called instructive theory holds that the antigen is brought to the locus of antibody synthesis and there imposes in some way the synthesis of the specific antibody with reactive sites which are complementary to the antigen.
The clonal selection theory, evolved by Burnett (1960), presupposes that the information requisite to the synthesis of the antibody is part of the genetics. While the body develops a wide range of clones of cells necessary to cover all antigenic determinants by random mutation during early embryonic life, those clones which are capable of reacting with antigens of the body ("self') are destroyed, leaving only those cells which are not oriented to self ("non-self'). Upon stimulation by a foreign antigen, the clones of the cells corresponding to the particular foreign antigen are stimulated to proliferate and to produce the antibody.
Other researchers demonstrated that there are at least four different antigens formed by descendants of a single cloned cell. By this mechanism, the information for antibody synthesis is contained in the genetic material of each cell (DNA) but is normally repressed. The antigen then assumes the role of a de-repressor and initiates (provokes) the RNA synthesis for a particular messenger, resulting in the corresponding antibody production. The antigen would instruct the genetically predisposed capability of multipotential cells as to which antibody to produce and might also command the cells to proliferate, resulting in clones of properly instructed cells.
There are two possible mechanisms for the elimination of antibodies against self: immunological nonresponsiveness and immunological paralysis. There are several states of immunological nonresponsiveness; one is illustrated by the exposure of a foetus or newborn to an antigen prior to the development of its ability to recognise the antigen as non-self (immunological incompetence). Immunological paralysis results from the injection of a very large amount of antigen into immunologically competent individuals. Nonspecific immunological suppression by cortisone, ACTH, nitrogen mustards and irradiation is also well known.
Cellular sensitivity, also known as delayed or cellular hypersensitivity, depends on the development of immunologically reactive or "sensitive" lymphocytes and possibly other cells which react with the corresponding antigen to give a typical delayed-type reaction after a period of several hours, days or even weeks.
Cellular hypersensitivity depends on the original antigenic stimulation and a latent period, and is specific in its response. Delayed-type hypersensitivity is characteristic of the body's response to various infectious agents such as viruses, bacteria, fungi, spirochetes and parasites. It is also characteristic of the body's response to various chemicals, such as mercury, endotoxins, antibiotics, various drugs and many other substances foreign to the body.
The induction of a hypersensitivity reaction requires the presence in the tissues of the whole organism or certain derivatives of it, in addition to the specific antigen such as a lipid in addition to tubercle bacillus protein. Sensitisation to a non-infectious substance must be mediated through the skin or mucuous membranes which probably provide further necessary co-factors.
A delayed hypersensitivity reaction may be enhanced experimentally by the employment of the antigen in a mineral oil adjuvant with added Mycobacterium tuberculosis or by injection of the antigen directly into the lymphatics. The delayed hypersensitivity response is accompanied by mild to severe inflammation which may cause cell injury and necrosis. The inflammatory response which occurs in delayed-type hypersensitivity may not be protective, and in many instances may even be harmful (e.g., rejection of grafts is directly linked to delayed hypersensitivity).
IMMUNOPATHOLOGY OF HYPERSENSITIVITY REACTIONS:
Immediate Hypersensitivity
This is the antibody-type reaction that is a secondary consequence to the beneficial effect of the combination of an antibody with its antigen.
Arthus-type Reaction
This reaction results from the precipitative union of a large amount of antigen with a highly reactive antibody in the blood vessels, and leads to vascular damage. The cascade of events includes spastic contraction of the arterioles, endothelial damage, formation of leukocyte thrombi, exudation of fluid and blood cells into the tissues, and sometimes ischemic necrosis. Periarteritis nodosa results from a similar antigen-antibody reaction and is characterised by inflammation of the smaller arteries and periarterial structures. it is accompanied by proliferation of the intima and two types of occlusion: (a) by proliferation or thrombosis; or (b) by the formation of nodules containing neutrophils and eosinophils.
Anaphylaxis
Injection of antigen and its combination with antibody may cause release from the cells (especially mast-cell fixed basophils) of physiologically active substances such as histamine, serotonin, acetyicholine, slow-reacting substances (SRS) and heparin. They act on smooth muscle and blood vessels and cause anaphylactic (hypersensitivity) shock, asthma attack, allergic oedema, rhinitis or hay fever, and accumulation of fluid in the joints.
Atopy
Atopy is caused by the union of antigen—usually pollens, dust, milk, wheat and animal danders—with a peculiar type of antibody (reagin). This reaction is relatively heat-labile and cannot be demonstrated by in vitro procedure. It has a special affinity for the skin and for familial predisposition to the disease. The reaction is nevertheless similar to other immediate-type sensitivities, with the release of histamine and its manifestation principally as asthma (breathing paralysis), hay fever, urticaria, angioedema and infantile eczema.
Delayed Hypersensitivity
The typical pathology of delayed hypersensitivity due to infectious agents involves perivascular infiltration of lymphocytes and histiocytes with the destruction of the antigen-containing parenchyma in the infiltrated area. The visual manifestations may vary from slight erythema and oedema to a violent reaction with progressive tissue destruction and necrosis. Local reactions include papular rose spots of typhoid fever, meningitis and a variety of infectious diseases, and contact sensitivities to plant and chemical substances manifesting as erythema, followed by papule and vesicle formation with resultant tissue damage and desquamation. Systemic reactions may accompany severe local reactions or may result from inhalation of the allergenic substances.
Humoral antibodies do not seem to play a role in delayed hypersensitivity reaction. The reactivity is transferred only by cells, presumably sensitised lymphocytes, and it is unlikely that histamine or other physiologically active substances play a role in the reaction. The reaction extends to any or all tissues where the offending antigen may occur.
Isoimmunological Disease
This is the result of an immunological reaction of a member of the same species to the tissue of another member of the same species. A blood transfusion reaction in a person given an incompatible blood type is a typical example. Another example is erythroblastosis fetalis, which results from the transfer of antibodies against the red blood cells of the foetus to the foetal circulation. Homograft rejection of tissues or organs between nonisologous members of a species is also immunologically based.
Immunological Disease Resulting from Adsorption of Foreign Substances
Under certain circumstances, foreign substances such as medications may combine with cells to render them antigenic. Subsequent exposure to such a foreign substance results in lytic, agglutinative or other types of cell-destructive activity. Such a reaction may involve red blood cells (drug-induced anaemias), platelets (drug-induced thrombocytopemc purpura), and leukocytosis (drug-induced agranulocytosis).
Bacteria or viruses may also alter cell surfaces by coating or by unmasking antigens through enzymatic activity which may render them vulnerable to immunological destruction.
Autoimmune Disease
Under certain circumstances, the body may respond immunologically to its own components or to intrinsic substances which are related antigenically to the host's own tissues. The circulating antibody or sensitised cells which are produced are then active in causing cellular injury to the tissues or organs of the body which bear the corresponding antigen.
Waksman (1962) proposed several mechanisms of autoimmunisation, such as:
1.Vaccination with organ-specific antigens which are isolated from the lymphatic channels and bloodstream and are not recognised as self when brought into contact with the immunologic process. They are represented in the central and peripheral nervous systems, lens, uvea, testes, thyroid (thyroglobulin), kidneys and other organs.
2.Vaccination against constituents of tissues which have been altered antigenetically by various factors. These include myocardial infarction, X-irradiation, enzymatic or other chemical alteration, and changes induced by infectious disease agents or by drugs. Erythrocytes, platelets and leucocytes are the most affected cells. Various organs may also be affected.
3.Vaccination with heterologous antigens which are sufficiently different to permit an immunological response but sufficiently alike to react with autologous antigens.
4.Alteration of the immunological apparatus so as to result in the failure of recognition of self. This occurs in neoplasia of the lymphatic system and in experimental grafting of immunologically competent heterologous lymphatic tissues under conditions which suppress the host's response to the graft and give rise to the wasting "runt disease" or "homologous disease".
5.Possible hereditary or other immunological abnormality. This is represented by a hyper-reactivity to antigens or other aberrations without apparent antigenic stimulation. Such mechanisms might be related to certain forms of the "collagen diseases", such as systemic lupus erythematosus in which there is an antibody against a diversity of antigens.
6.Experimentally, Freund's mineral oil adjuvant (usually with added mycobacteria) and certain bacteria or bacterial toxins may so alter the host as to bring about a ready response to unaltered normal homologous tissue. These "experimental autoallergies" include a wide variety of organs and tissues, and are now being employed as model systems for investigation of autoimmune phenomena.
Both humoral antibody and sensitised cells may function in autoimmune disease. Auto-antibodies seem to be involved in reactions with cells which are easily accessible, such as the formed elements of the blood (in haemolytic anaemia, leucopeni thrombocytopenia), vascular endothelium, vascular basement membrane including the glomerulus (in acute glomerulonephritis and ascites cells (neoplastic immunity).
Production of lesions in the solid vascularised tissues appears to depend on delayed hypersensitivity reactions with sensitised lymphoid cells (such as in allergic encephalomyeitis, thyroiditis, subacute and chronic glomerulonephritis, orchitis, adrenalitis and many other diseases).
It is quite obvious now that the same autoimmune mechanisms are responsible for the same diseases in human beings and that the extent of such damage is enormous and keeps increasing with more and more vaccines added to to "recommended" schedule.
Indeed, vaccines such as the pertussis vaccine are actually used to induce autoimmune diseases in laboratory animals, the best and most publicised example being the so-called experimental allergic encephalomyelitis (EAE). When, as expected, these unfortunate animals develop EAE from the pertussis vaccine, the causal link is never disputed; yet when babies after vaccination with the same vaccines develop the same symptoms of EAE as the laboratory animals, the causal link to the administered vaccine is always disputed and usually considered "coincidental". Lately, innocent parents and other carers have been accused of causing the symptoms of vaccine darn age by allegedly shaking their babies.
Systemic lupus erythematosus is one of the innumerable recognised side effects of a number of vaccinations. One of the best papers (if not the best on this is by Ayvazian and Badger (1948), and it has not lost any of its punch and relevance since it was published. They describe three cases of nurses who were literally vaccinated to death. The authors surveyed a group of 750 nurses who trained at a large municipal hospital between 1932 and 1946, and detailed the cases of three nurses who were vaccinated with a multitude of vaccines over a period of time and developed and succumbed to disseminated lupus erythematosus.
Typically, these nurses were given the following tests and vaccines in short succession: the Schick test; three days later, the Dick test; seven days later, typhoid-paratyphoid vaccine; seven days later, another typhoid-paratyphoid vaccine (a double dose); seven days later, the third typhoid-paratyphoid vaccine; and seven days later, the fourth typhoid-paratyphoid vaccine. Every time, the recipient developed local erythema and/or fever and malaise, but it did not deter the doctor from administering yet another series of vaccines, starting only 14 days after the first lot of tests and typhoid-paratyphoid vaccines.
This time, after all these injections, one of the trainee nurses was given her first injection of scarlet fever streptococcus toxin with "no ill results". One week later, she was given the second injection of streptococcus toxin, after which she developed joint pains and fever. She did not report these reactions to the health office. Nine days later, she returned and received the third injection of a fourfold dose of streptococcus, after which she developed severe arthralgia in the fingers and knees and a sore throat.
She was hospitalised for five days and discharged with the diagnosis "Dick-toxin reaction". Only five days later her inoculations were continued, first in lower and then in gradually increasing doses so that the series included a total of 10 instead of the usual seven injections. Epinephrine was administered with each of these injections of streptococcus toxin and toxin-antitoxin.
Two months after the last lot, the trainee nurse was re-admitted to the hospital with swelling and pain of the ankles and toes and tenderness of the joints of both hands, which had been constant since the first Dick test five months earlier. The diagnosis was "rheumatic arthritis". She was given aspirin, but two weeks later the pain came back and she developed chills and fever, sore throat and cough. One month later, the trainee nurse was re-admitted to hospital for two weeks, and during this admission a streptococcus vaccine was started in small doses, but because of her severe reaction "further vaccines were refused". The diagnosis after this admission was "rheumatoid arthritis and infectious mononucleosis". Four months later, the trainee nurse noticed skin eruptions over her nose and both cheeks, and her saliva became foul. The skin and cheeks, upper lips and the bridge of the nose were covered with purplish red, mottled and indurated rash eruptions. Two months later, the eruptions spread over much of the body. A year later, the trainee nurse died, but not before developing severe symptoms of high fever, tachycardia, diarrhoea and showing abnormal blood tests.
It was not enough that this unfortunate trainee nurse died; there were another two cases reported, almost identical to the first case. We shall never know bow many of the remaining 747 trainee nurses developed less lethal, but still health-incanacitating. reactions.
If someone said that this type of "medical treatment' had been given to the inmates of the Nazi concentration camps, I would not be surprised. However, this type of "medical treatment" was and is being given with impunity to millions of babies, children, teenagers and adults in so-called free and democratic countries as well as in the Third World. Meanwhile, the health authorities refuse to accept that vaccines cause such reactions and even deaths.
VACCINATION: A SAFETY WARNING
The conclusions which follow the study of relevant medical and immunological literature dealing with vaccines and the adjuvants used in vaccines is that the absolute safety of these substances can never be guaranteed. According to Gupta et al. (1993), the toxicity of adjuvants can be ascribed in part to the unintended stimulation of various mechanisms of the immune response. That's why the safety and adjuvancy must be balanced to get the maximum immune stimulation with minimum side effects.
My conclusion is that such balance is impossible to achieve, even if we fully understood the immune system and the full spectrum of deleterious effects of foreign antigens and other toxic substances such as vaccine and drug adjuvants and medications on the immune system of humans, and particularly on the immature immune system of babies and small children. Injecting any foreign substance straight into the bloodstream will only cause anaphylactic (sensitisation) reactions. Nature, over thousands and thousands of years, has developed effective immune responses; yet man, without respect for nature, demonstrably causes more harm than good.
Vaccination procedures are a highly politically motivated non-science, whose practitioners are only interested in injecting multitudes of vaccines without much interest or care as to their effects. Data collection on reactions to vaccines is only paid lip service, and the obvious ineffectiveness of vaccines to prevent diseases is glossed over.
The fact that natural infectious diseases have beneficial effect on the maturation and development of the immune system is ignored or deliberately suppressed.
Consequently, parents of small children and any potential recipients of vaccines and any orthodox medications should be wary of any member of the medical establishment (which is little more than a highly politicised business system) extolling the non-existent virtues of vaccination. Even though Australian law requires doctors to warn patients about all side-effects of all medications and procedures of a material nature, whether the patient asks or not, doctors as a rule do not uphold this important law.
References (in alphabetical order)
• Aprile, M.A. and Wardlaw, A.C., 1966. Aluminium compounds as adjuvants for vaccines and toxoids in man: A review Can. J. Public Health 57:343.
• Asa, PB., Cao, Y. and Garry, RF., 2000. Antibodies to Squalene in Gulf War Syndrome. Experimental Molecular Pathology 68:55—64.
• Ayvazian, L.F. and Badger, TL, 1948. Disseminated lupus erythematosus occurring among student nurses. New England Journal of Medicine 239(16):565—570.
•Bizzini, B., Carlotti, M. and Fattal-German, M., 1992. Lnduction of various cytokines in mice and activation of the complement system in rats as a part of the mechanism of action of the Corynebacterium granulosum-derived P40 immunomodulator. FEMS Microbiol. Immunol. 105:17 1.
• Burnett, F.M., 1960. Theories of immunity. Persp. Biol. Med III:447—458.
• Butler, N.R., Wilson, B.D.R., Benson, P.F., Dudgeon, J.A. at al, 1962. Response of infants to pertussis vaccine at one week and to poliomyelitis, diphtheria and tetanus vaccine at six months. Lancet ii:112.
• Chedid, L, 1985. Adjuvants of immunity. Ann. immunol. (Inst. Pasteur) 136D:283.
• Coursaget, P., Yvonnet, B., Relyveld, E.H., Barres, JL. at al., 1986. Simultaneous administration of diphtheria-tetanus-pertussis-polio and hepatitis B vaccines in a simplified immunisalion programme: immune response to diphtheria toxoid, tetanus toxoid, pertussis and hepatitis B surface antigens. Infect, immunity 51:784.
• DeVries, P., Van Binnendijk. RS., Van der Marel, P., Van Wezel, A.L. et al, 1988. Measles virus fusion protein presented in an immune-stimulating complex (ISCOM) induces hemolysis-inhibiting and fusioninhibiting antibodies, virus-specific T-cells and protection in mice. J. Gen. Virol. 69:549.
• Dolin, P.J., Faal, H., Johnson, G.J., Minassian, D. at aL, 1997. Reduction of trachoma in a sub-Saharan village in absence of a disease control programme. Lancet 349:1511—1512.
• Friedwald, W.F., 1944. Adjuvants in immunization with influenza virus vaccines. J. Exp. Med 80:477—491.
• Glenny, A.T., Buttle; G.A.H. and Stevens, M.F., 1926. Rate of disappearance of diphtheria toxoid injected into rabbits and guinea pigs: toxoid precipitated with alum. J. Pathol. Bacteriol. 34:267.
• Grayston, J.T., Wang, S.P., Woolridge, R.L. and Alexander, ER., 1964. Prevention of trachoma with vaccine. Arch. Environ. Health 8:518—526.
• Gregoriadis, G., 1976. The carrier potential of liposomes in biology and medicine (first of two pasts). New Eng. J. Med. 295:765.
• Gupta, R.K., Relyved, ER, Lindblad, EB., Bizzini, B. at al., 1993. Adjuvants - a balance between toxicity and adjuvanticity. Vaccine 11(4).
• Henle, W. and Henle, G., 1945. Effect of adjuvants on vaccination of human beings against influenza. Proc. Soc. Exp. Biol., NY 59:179—181.
• Hilleman, M.R., 1966. Critical appraisal of emulsified oil adjuvants applied to viral vaccine. Prog. in Med. Virology 8:131-182.
• Lovgren, K. and Morem, B., 1990. The ISCOM: An antigen delivery system with built-in adjuvant. Mol. immunol. 28:285.
• McLaughlin, CA, Schwartzman, S.M., Homer, B.L., Jones, G.H. at al., 1980. Regression of tumors in guinea pigs after treatment with synthetic muramyl dipeptides and trehalose dimycolate. Science 208:415.
• Miller, L.F., Peckinpaugh, R.O., Adander, T.R., Pierce, W.E. at al, 1965. Epidemiology of prevention of acute respiratory respiratory disease in naval recruits: II. Efficacy of adjuvant and aqueous adenovirus vaccines in prevention of naval recruits respiratory disease. Am. J. Public Health 55:47—59.
• Morein, B., Fossum, C., Lovgren, K. and Hoglund, S., 1990. The ISCOM: a modern approach to vaccines. Semin. Virol. 1:49.
• Pittman, M., 1984. The concept of pertussis as a toxin-mediated disease. Pediatric infectious Diseases 3(5):467—486.
• Salk, J.E., 1951. Use of adjuvants in studies on influenza vaccination. 3. Degree of persistence of antibody in human subjects two years after vaccination. JAMA 151:1169—1175.
• Salk, J.E., Lewis, L.J., Younger, J.S. and Bennett, B.L., 1953. The use of adjuvants to facilitate studies on the immunologic classification of poliomyelitis viruses. Am. I. Hyg. 54:157—173.
• Wakaman, B.H., 1962. Auto-immunization and the lesions of auto-immunity. Medicine 41:93—141.
Many research projects on new vaccines against life-threatening diseases, such as malaria, TB and HIV, as well as neglected tropical diseases, have, therefore, been conducted with nonoptimized adjuvants. This is particularly true for R&D carried out within the public sector or by small biotechnology companies. These organizations may be tempted to simply use alum that induces only strong antibody responses, or water-in-oil emulsions, which have safety and manufacturing concerns. Such overly pragmatic approaches may result in otherwise viable antigens being abandoned as candidates for new vaccines and, consequently, result in a significant waste of resources from public and private domains.
Therefore, the challenge is to establish a system that provides open access to adjuvants and adjuvant information to nonprofit initiatives, without inflicting on the freedom-of-operation of the owner of the adjuvant.




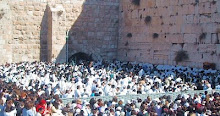




No comments:
Post a Comment